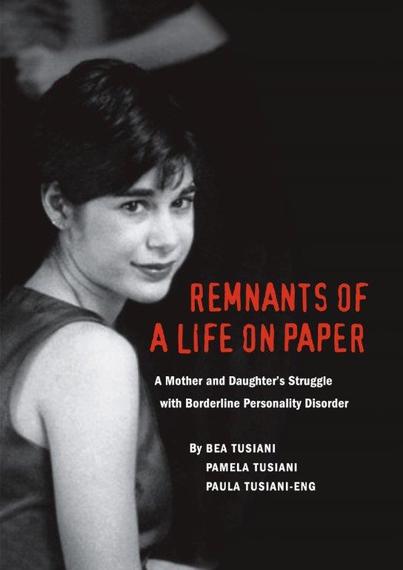
Remnants of a Life on Paper: A Mother and Daughter's Struggle with Borderline Personality Disorder
By Bea Tusiani, Pamela Ann Tusiani & Paula Tusiani-Eng
A Book Review by Dr. Lloyd Sederer
If you are looking for reasons to believe in God, they abound in this book.
If you are looking for reasons not to believe in God, they abound in this book.
I knew the outcome of the Remnants of a Life on Paper, having heard it from the mother, Bea Tusiani, whom I met recently for the first time at a psychiatric meeting in NYC. Yet this book was still a page-turner of a memoir -- written, compiled and told with utter candor and generosity by a mother who lost her 23-year-old daughter. We accompany, for 2.5 years, a family's nightmarish struggle from the time their 20-year-old child became acutely ill with a common mental disorder -- about which we know far too little about its pathogenesis and even less about how to master its destructive symptoms and debilitating psychic confusion.
Personality disorders, by definition, are disturbances of character that begin in adolescence and form the ongoing basis of how a person feels, thinks and behaves. These disorders are not transient: They are enduring and exceedingly difficult to change. Borderline personality disorder (BPD) is one of these character disturbances: people affected show a myriad of often changing symptoms (which can make diagnosis difficult, at first) including intense mood swings; impulsivity leading to often horrific judgment and self-destructive behaviors; chaotic relationships driven by urgent needs for attachment, yet an inability to tolerate closeness and dread of abandonment; episodes of loss-of-reality testing (where psychotic symptoms transiently appear); profound difficulties maintaining a sense of identity (who am I?); and commensurate problems in tolerating living in one's own skin. Frequently, alcohol and drug use and abuse, and anorexia and bulimia accompany BPD and add to a person's turmoil and treatment challenges.
Here is how Pamela Tusiani put it (p. 144):
The demon nests inside me.
When it wakes, I fall into a trance of violent paranoia.
Blue and yellow pills line up at full attention.
Tempted by distaste,
My heart pumps with thick muddy rage.
BPD is twice as common as schizophrenia and bipolar illnesses (combined), with likely more than 10 million people in the USA impacted (2 to 6 percent of the adult population). Women are more frequently diagnosed with this condition, but they are not alone in experiencing it. BPD disproportionately represents psychiatric inpatient and outpatient statistics, perhaps because of how the internal turmoil of the condition generates external chaotic and destructive behaviors.
Pamela was the third child of native New Yorkers and an honors college student at Loyola College when she was first hospitalized at the Johns Hopkins Medical Center psychiatric unit in 1998. Experienced doctors then said she was depressed and that treatment would help her in a matter of weeks. But the depression was the tip of the iceberg, or maybe an indication of the hell brewing inside. She did not promptly recover. She left school, returned to NYC, had multiple hospital stays and 12 ECT treatments before the diagnosis of BPD was made. She was often suicidal, took overdoses of pills and cut herself frequently and deeply. After five months and five hospitalizations she seemed to be doing worse, not better.
Her parents, Bea and Mike, are impressively resourceful people. With their unrelenting support and advocacy Pamela was admitted to Austen Riggs, a long-term, open psychiatric treatment center that focuses on providing intensive psychotherapy. It is set on a small campus of residential buildings located in the semi-rural New England town of Stockbridge, Massachusetts. She spent 19 non-consecutive months there, as her parents paid out of pocket the tens of thousands of dollars it cost each month. Riggs proved that it "has more freedom than she can handle." (p. 94). The clinical leadership at Riggs said she had to leave and recommended (what evidently they believed) to be an accredited program for people with "dual diagnoses," i.e., psychiatric and substance-use disorders, in Malibu, California, called Road to Recovery. This program was equally financially demanding and 3,000 miles away from family and home.
Pamela's course at Road to Recovery was labile, with times of sobriety and rebuilding her life and times of falling into states of impulsivity and self-abuse. She developed seizures, which proved to be "psychogenic," meaning that it was her psychology, not her neurology that produced them. Such is the power of the mind.
People with BPD have limited responses to psychiatric medications, and many drugs (of a variety of classes) were tried on Pamela -- but her depression, anxiety, distortions of reality and impulsivity prevailed. The side effects of these drugs, alone or in combination, can be unbearable, especially if benefits are minimal: weight increases, fatigue is constant, libido evaporates, concentration is very hard, and dizziness an ever-present threat. Over two years after her first episode of illness, her mother read about a medication called Parnate, a drug that I used a great deal until the serotonin drugs (like Prozac and Paxil) came along in the 1990s. Parnate is in the class of anti-depressants called monoamine oxidase inhibitors (as is Nardil), and has been shown to be helpful in "atypical depressions," the type of mood states that people with BPD can have. Pamela spoke with her prescribing psychiatrist affiliated with the California program about Parnate and she began to take it. That the medication, however, left her vulnerable to a known, serious adverse effect, to which she succumbed -- likely unnecessarily so.
I believe all behaviors serve a purpose. They may not make sense at first, but they are "solutions" (p. 219) to severe psychic states that demand response or relief. Cutting is a good example, where the act can seem senseless but instead it quiets (transiently) emotional pain and self-loathing. Compulsive sexuality or drug intoxication also serve purposes, which are vital to understand if a person is to find other, less destructive, answers to their compelling distress. The long-term treatment of mental disorders (including BPD), when done well, involves helping a person understand their experience and find alternate methods of mastery. Pamela was well into her journey of recovery when a series of treatment program and medical errors conspired to kill her. The awful irony was that she did not take her life, but irresponsible, stigmatizing and poor residential and medical care did.
One of the moments, and there are many in the closing pages of this book, that gives me shame about how professionals and administrators do not meet their responsibilities, was in the Emergency Room at UCLA medical center. Pamela had been brought there after experiencing a known hypertensive drug reaction induced by eating certain types of cheese while taking Parnate. The reaction is characterized by very high blood pressure with confusion, headache and restlessness. But instead of those serious symptoms being recognized, her clinical state was attributed to her being a drug user, a "mental patient," and she was put on suicide watch. The result was that she did not receive the proper medical evaluation and care that might have spared her life. This is disturbingly common today, over 10 years later, as reported in medical reports of psychiatric patients being segregated and not getting proper attention for heart, lung or other problems that prompted their emergency visit. Many don't say they have a psychiatric condition to prevent this from happening.
Other moments that made me cringe were told with clarity and intelligence throughout the book.
Among the most disturbing are examples of demonizing parents of a person with a mental illness or blaming the victim (of rape, for example) because she has a psychiatric condition. Reading about what appears to have been a coverup of wrong doing in the California residential program was enraging for me. Imagine what that was like for her parents and siblings. Having been the medical director of McLean Hospital, a Harvard psychiatric teaching hospital, and a government official for more than 12 years, I believe everything depicted in this profound book is not only possible, but happens more than we want to think.
The story of Pamela and her family's labors and love for each other is told in alternating prose by Bea, the mother, and "remnants" from Pamela's journals, which she appears to have faithfully kept and are given to us in spare and thoughtful segments as time goes by. There are also vivid paintings and drawings by Pamela at various stages of her short life from the time she became acutely ill. These are emblematic of her demons as well as illustrative of her creative talents.
Paula Tusiani-Eng, another daughter in their family, is also listed as author. She was instrumental in the legal work and in giving the story its first-person voice. This book is a family affair -- surely one way they have worked to recover and to help others similarly affected.
But I am most admiring of Bea. As has been said, no parent, no mother, should see a child die. And to lose a child who may have recovered is all the more agonizing. Bea Tusiani only tells us at the end of the book that she is a writer -- though it is plain enough how powerful a writer she is as she lets the story, the events she chronicles, show us so much about her daughter, her family, and our flawed mental health and medical systems. What is also so inspiring about the book Bea Tusiani has given us, which is why I found hope (reason to believe), is how she gives us a front-row seat, so we witness the courage, love, determination and stamina of the Tusiani family. I am sure that Pamela would be proud to see how her pain, spirit and resilience -- and that of her loved ones -- have been so sensitively and cogently captured in these "remnants ...on paper."
---
 Dr. Sederer's new book for families who have a member with a mental illness is The Family Guide to Mental Health Care (Foreword by Glenn Close).
Dr. Sederer's new book for families who have a member with a mental illness is The Family Guide to Mental Health Care (Foreword by Glenn Close).
Dr. Sederer is a psychiatrist and public health physician. The views expressed here are entirely his own. He takes no support from any pharmaceutical or device company.
www.askdrlloyd.comhttp://www.askdrlloyd.com